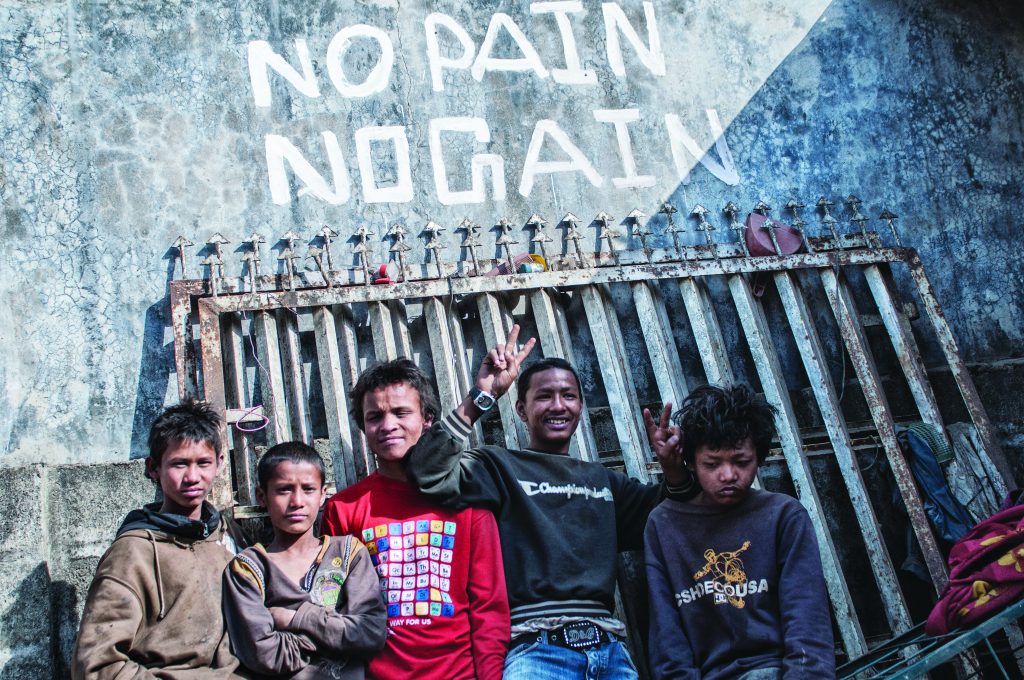
Nepalese migrant workers are most at risk of contracting HIV. Without proper screening and information, this poses a worrying threat for the rest of the population
Text Zigor Aldama
Photos Zigor Aldama and Miguel Candela
Ram Lalita didn’t know that she had been infected with HIV until AIDS killed her husband. “He got very sick suddenly, so we took him to a shaman. He performed a ritual and recommended taking herbs, but it didn’t work. Finally, we had to take him to the hospital,” Lalita, who is in her forties, recalls.
Lalita and her husband had to spend a relative fortune to seek help, and travelled 50 kilometres along
the bumpy roads of eastern Nepal to get to the nearest health facility – but all in vain.
At the Mahottari Hospital, a shocking truth was revealed: Lalita’s husband, a migrant worker who used to have a job as an electrician in India, had had intercourse with HIV-positive prostitutes in the northeastern Assam state. “He sent money from there and used to come back home about three times a year,” she says, trying to hold back her tears.

The retroviral pills she takes now keep her alive and are provided free of charge by the Nepalese government. However, fighting the disease is not her sole hardship; fighting stigma and poverty are additional burdens.
“After the death of my husband, I lost my income. So we sold the land we owned to feed ourselves and we went back to my parent’s home. I tried to conceal the true reason of his death, but soon all in the village knew.”
As a result, her family expelled them from their home, and parents in the town forbade their kids from playing with Lalita’s two sons – even though they were confirmed HIV-negative. She now lives in a rudimentary hut and has to wash her clothes and utensils far from the stretch of river where others do the same. She has been completely alienated and survives on charity.
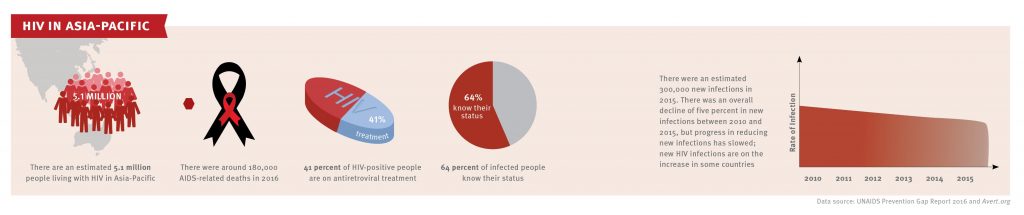
Unfortunately, she is not the only one. Nepalese migrant workers, especially those travelling to other South Asian countries for work, are at the highest risk of becoming infected with HIV on the continent. The general lack of checks and healthcare access in the most remote areas makes it difficult to assess care and treatment.
The Community Development Project (CDP), a local NGO sponsored by Action Aid, surveyed 600 migrant workers in six districts and found that five percent had contracted the virus. None of the people surveyed suspected that they were infected.
“That’s a lot given the fact that many refuse to take the tests – especially for those who paid for prostitutes,” says Biyay Kumar Chaudhary, the current president of the CDP. “So we have started a campaign to request that women refrain from having sex with their husbands upon their arrival until they have been checked.”
Unfortunately, in Nepal, women don’t have a say. “That will make many HIV-positives remain in the shadows until it’s too late,” Chaudhary explains.
We have started a campaign to request that women refrain from having sex with their husbands upon their arrival until they have been checked.
–Kumar Chaudhary, president of the Community Development Project
According to statistics from UNAIDS, migrant workers comprise around 10 percent of the global HIV-positive population – almost the same percentage as homosexuals, and far higher than the four percent of drug users. “They are also bringing the virus to the low-risk population, because they’ve become the main source of infection for women who do not engage in sex work, which already make up 30 percent of the total HIV-positive population,” says Nafisa Binte, Unicef Nepal’s AIDS programme director.
According to the latest national statistics (in July 2016), 28,865 people live with the disease in the country. However, UNAIDS estimates put the number as high as 46,000; Unicef estimates that it is as high as 65,000. About 4,000 children under the age of 14 have also been infected, and have developed the disease.
Sex workers are suffering the worst. Bimila Panday knows that well. She became a prostitute out of desperation. “My husband left for India to work, and he disappeared for eight years. We knew nothing, so we assumed the worst. I had no way to make a living without his support, so I started to have sex with men who paid for it,” she recalls.


Although she knew the risks, she was forced to have unprotected sex by some of her clients, many of whom were migrant workers who had returned home. “Most people don’t know what AIDS is, and, obviously, how to avoid it.
So there were times when I had to agree to unsafe sex,” she says.
She has paid dearly for it. She got infected, and has no way of knowing, let alone contacting, the person who infected her. The disease killed her husband sometime after he returned to Nepal, and his family blames her for his death – in fact, the whole town does.
“I have no way to tell if I infected him or he infected me, because he died just months after his return,” she says. Either way, she was forced to flee and find shelter at the CDP.
Most people don’t know what AIDS is, and, obviously, how to avoid it. So there were times when I had to agree to unsafe sex.
–Bimila Panday, former sex worker, AIDS sufferer
She got lucky: Thanks to the NGO, she abandoned sex work and is now an advocate for safe sex among prostitutes. “We have to do something, because if we don’t, the epidemic will strike back,” she says.
The problem, Binte explains, is that “everybody in Nepal can become a migrant worker at some point, which makes it extremely difficult to screen the population.”
Nepal shares a 1,850 kilometre-long border with India, and citizens of both countries don’t need a visa to visit, or work in, the neighbouring country, so migrant work is common.
“This migration pattern is very different from that of the West. Most trips are temporary and linked to specific circumstances, like a drought,” says Binte.

Related: An Invisible Disease
Related: The Silent Epidemic
Related: They Call it Happyland
Ram Bahadur Gotami is a good example. He left his small village near Pokhara because of a disastrous harvest, and returned in very bad shape just a few months later. He’d lost a lot of weight, and suffered constant headaches. He was admitted to the Western Regional Hospital. His doctor, Basand Tamprakar, decided to run a series of tests. They brought him bad news.
“He is suffering from clinical stage three of AIDS, so it will be very difficult to save his life,” Dr Tamprakar explained at the time of the interview.

But Ram had no idea what that meant. He had never heard of AIDS, and believed everything would be cured with pills. With increasing anxiety, he waited for a nurse to explain the situation and to offer psychological comfort.
“The lack of knowledge is deadly,” Dr Tamprakar says. “From 1,162 admitted HIV-positive patients, over 500 have got antiretroviral medication. But 170 have died. They seek help too late.”
An additional problem is that patients require a high-protein diet, which is hard to come by in Nepal. Previously, NGOs supported programmes by providing assistance in the form of dietary support, but with the international economic crisis, donations have slumped. In the West, AIDS is widely considered a chronic disease, so it receives much less attention; people would rather donate their money to other programmes.
The lack of knowledge is deadly. From 1,162 admitted HIV-positive patients, over 500 have got antiretroviral medication. But 170 have died. They seek help too late.
– Dr Basand Tamprakar, Western Regional Hospital, Nepal
And that’s how the vicious circle of AIDS keeps turning in Nepal. Unaware of the risks, countless migrant workers engage in unprotected sex with prostitutes working abroad in South Asia or the Middle East. Unaware of their infection, they return to their spouses, and pass on the infection, which can also then spread to their newborn babies. A lack of proper healthcare combined with social stigma makes it much worse.
In total, more than 5,000 people have died of AIDS in Nepal since the first case was diagnosed in 1998. Still, 70 percent of the population doesn’t yet know anything about it.

In 2015 the country launched its “Ending AIDS by 2030” programme, and UNAIDS applauded the initiative. However, the statistics provided in the 2015 report are not very encouraging. Only 26.5 percent of male respondents in a UN and government survey admitted to using a condom during “higher-risk sex”, and only four percent of the population has been tested for HIV. The mother-to-child transmission rate remains high at 35.7 percent.
Fortunately, campaigns have led to a 90-percent increase in safe sex practices among sex workers, and
58 percent have tested for HIV. Overall, UNAIDS believes Nepal is moving in
the right direction. “The new infection estimates also suggest that the trend of annual new infection is declining and will continue to drop further if the same level of intervention is maintained. The annual new infection cases is expected to decline to 899 by 2020,” the latest annual report reads.
But UNAIDS warns: “Even a small prevalence of HIV in the large population of male labour migrants, which is estimated at a staggering 505,728, obviously translates into a large number of people living with HIV”. Nepal still has a long way to go – and a lot of work to do.
For more stories from this issue, get your copy of Asian Geographic Issue 127, 2017.